Low-cost bone graft for bone reconstruction
Faculty: Prof. Jayesh Bellare, Chemical Engineering
Tata Fellow: Deepak Gupta (2014-16)

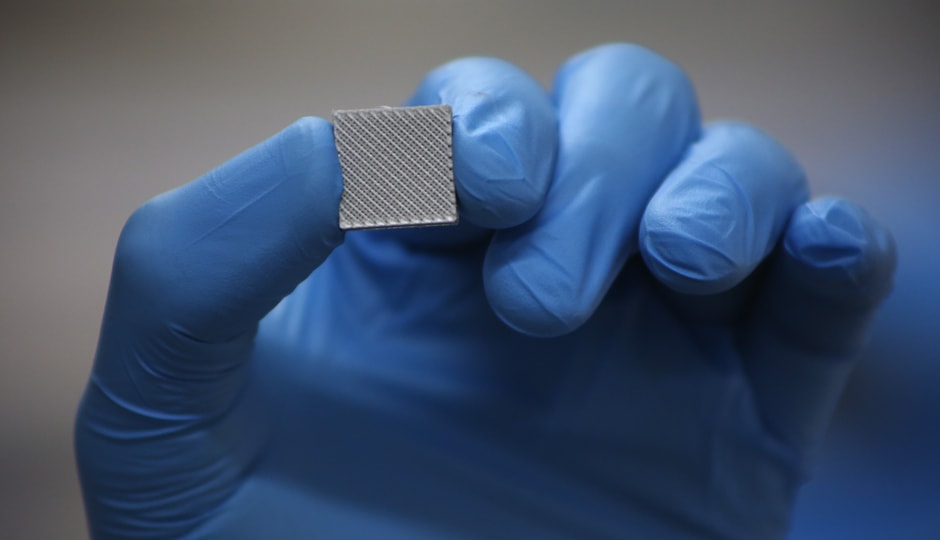
This project addresses the problem by bringing universal and customized bone graft which will not only eliminate the use of autograft with the second surgical site but will also bring down the cost and healing time, thereby benefitting 2 per cent of the total Indian population suffering from bone voids. Also, maxillofacial and orthopaedic surgeons have shown great interest in such products to be developed. There are various methods of preparation techniques of scaffolds like phase separation, particulate leaching, fiber bonding, electro-spinning, gas foaming, 3-D printing and others. In this work, 3-D printing from the fused deposition modeling technique is used with bio-compatible and bio-resorbable polymers for scaffold fabbrication. 3-D printing has allowed us to customize micro-porosity in terms of pore size, pore shape and overall porosity by modifying the internal structure and the interconnectivity among the pores of the scaffolds. The designs are created using Solidworks software and Python programming to generate the .gcode file for 3-D printing. Micro-porous scaffolds have been prepared using filaments of different polymers and different porosities can be incorporated into the same scaffold. A filament extruder is used to extrude the filaments out of polymeric beads. Characterization of the scaffolds has also been performed which includes TGA analysis, mechanical testing, porosimetry and bio-compatibility test. In the future, we will be using different blends of polymers for printing the scaffolds.

